A 70-year-old man was transferred to our department of nephrology for the evaluation of persistent fever and azotemia. He has been treated with anti-tuberculous (Tb) medication for Tb pleurisy in recent weeks. The laboratory findings at transfer were as follows: white blood cells, 25,030/mm
3; hemoglobin, 11.8 g/dL; platelets, 545,000/mm
3; C-reactive protein, 13 mg/dL; protein/albumin, 6.1/2.6 g/dL; blood urea nitrogen, 28 mg/dL; and creatinine, 2.06 mg/dL. Urinalysis showed both proteinuria (4+) and hematuria (4+). Serologic markers including immunoglobulin and complements were within normal range, except that myeloperoxidase anti-neutrophil cytoplasmic antibody (ANCA) was positive. On suspicion of ANCA vasculitis, 500-mg methylprednisolone was administered. While planning renal biopsy, the patient complained of severe right flank pain, and his hemoglobin level decreased from 11 to 7 g/dL. Abdominopelvic computed tomography showed kidney rupture with a subcapsular hematoma, and renal angiography revealed innumerous punctate contrast staining and a minute leak in the vascular bed of right renal artery (
Fig. 1); total embolization of the right renal artery was thus performed. After 2 days, a decrease in hemoglobin to 2.5 g/dL occurred. A focal contrast extravasation arising from the right gonadal artery was seen on further abdominal aortography; this culprit vascular branch was embolized again (
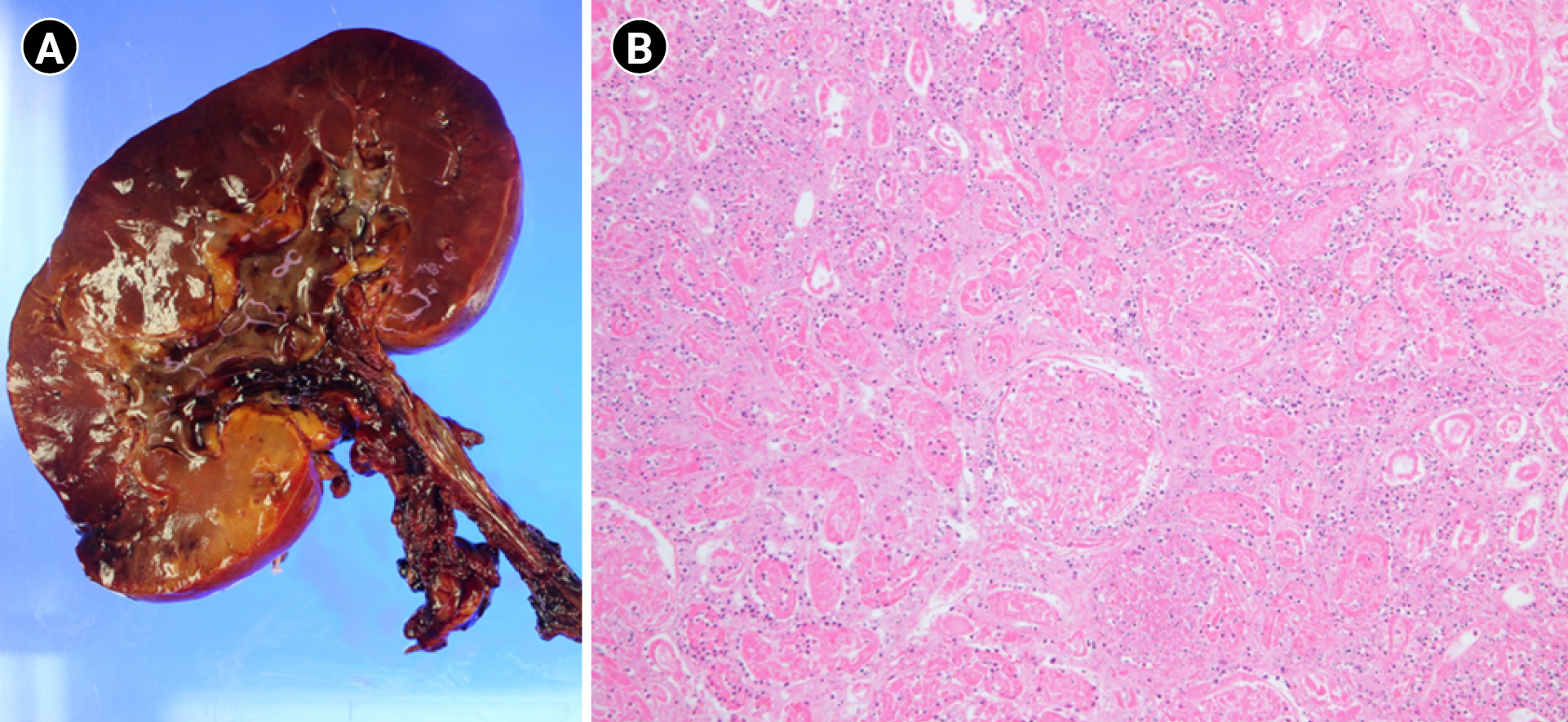
Fig. 2). Thereafter, right nephrectomy with hematoma evacuation was done. Macroscopically, the excised kidney revealed diffuse hemorrhagic infarct, and microscopically showed total ischemic necrosis with suspected diffuse vasculitis (
Fig. 3). Under a diagnosis of microscopic polyangiitis based on serology and histology, steroid, intravenous immunoglobulin, plasmapheresis, and continuous renal replacement therapy were applied. Taking cyclophosphamide after stabilization, he recovered enough to survive without dialysis. Creatinine level was around 2 mg/dL prior to discharge.
ANCA-associated vasculitis mainly involves small blood vessels, but can also rarely involve the middle arteries, which may be fatal if diagnosis and treatment are delayed. In the case of fever of unknown origin and renal impairment, this type of vasculitis should be considered in differential diagnosis.










 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print















